Teaming for Interdisciplinary Research Pre-Seed Program
Gut Microbial Therapy for Traumatic Brain Injury
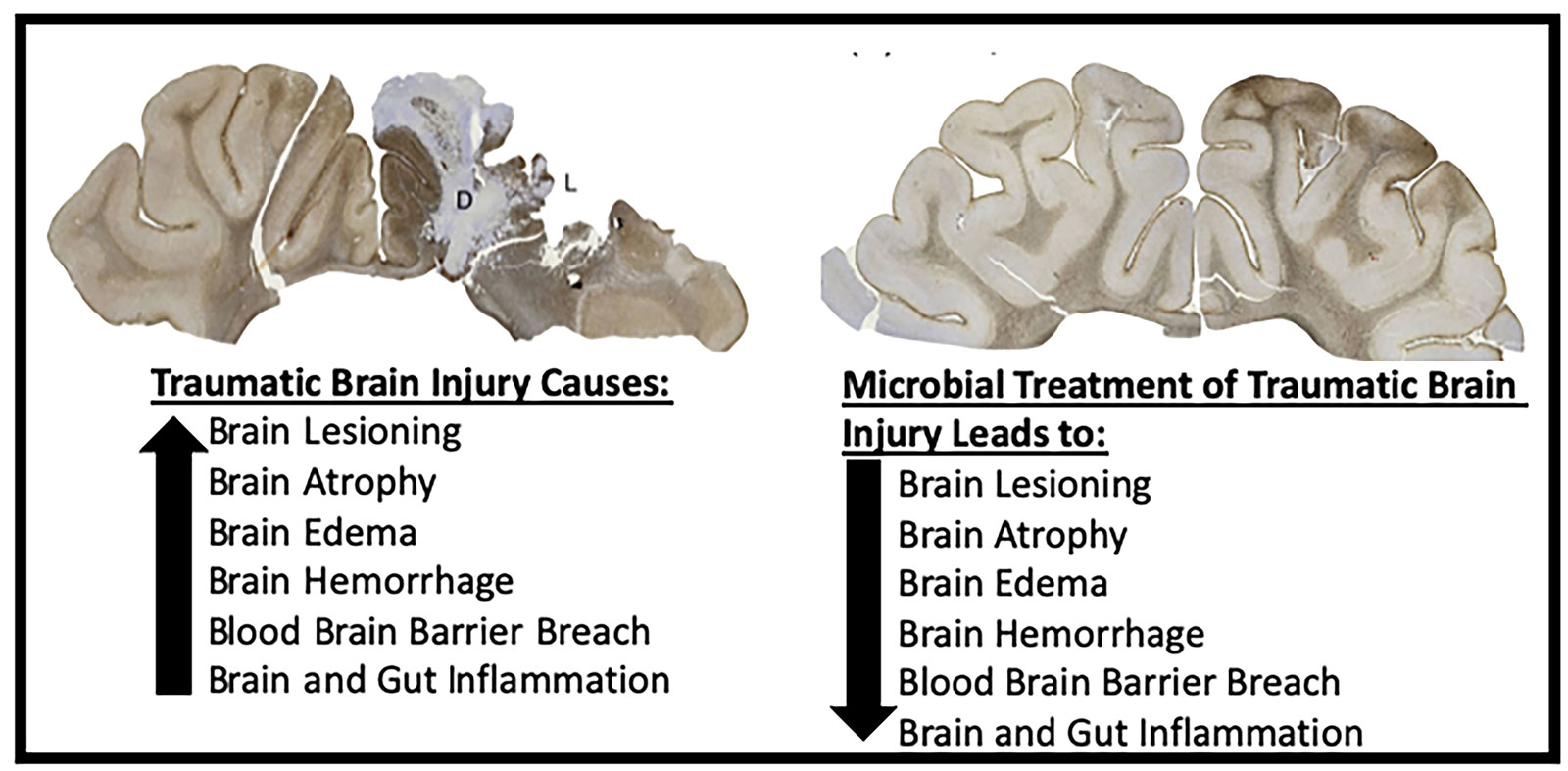
Each year 2.53 million Americans visit the emergency department after suffering a traumatic brain injury (TBI), of which 56,800 die. TBI is a major contributing factor to a third of all injury related deaths in the US. Hospitalization, rehabilitation programs, and long- term supportive care of over 288,000 TBI patients each year, are major contributing factors to the $76.5 billion in annual TBI medical costs. Despite TBI being a major health problem, there is currently no Food and Drug Administration (FDA) approved treatment for TBI. Acutely, TBI leads to a complex pathophysiology including the activation of the immune system resulting in increased brain lesioning and breakdown of the blood brain barrier leading to edema and hemorrhage that result in elevated intracranial pressure and brain herniation. There is close communication between the brain and gut through the microbiota-gut-brain axis (MGBA). In the gut, TBI typically causes breakdown of the intestinal wall, leakage of intestinal contents into the blood stream and an increase in systemic inflammation, and a decrease in normal healthy bacteria and an increase in bacteria commonly associated with disease. These changes in the gut negatively affect the brain resulting in increased brain damage, deficits in motor function, cognition, behavior and mortality.
Our research team seeks to take advantage of this close communication between the brain and gut by modulating the MGBA using novel microbial therapeutic bacteria to treat TBI. Preliminary studies have shown that microbial treatment leads to decreased neural cell death, edema, breakdown of the blood brain barrier and correlates with improvements in neurological severity scores in rodent TBI models. These promising initial results have led our research team to focus on 1) systematic identification of potential TBI therapeutic target bacteria and 2) compare the efficacy and safety of individual bacteria in a translational TBI pig model. The identification of effective bacteria that can modulate the gut microbiome after TBI leading to reduced brain injury and functional deficits has significant potential to improve the quality of life of millions of TBI patients each year.
Team Lead
Franklin West
Animal and Dairy Science / Regenerative Bioscience Center
westf@uga.edu
Team Members
Hea Jin Park
Department of Foods and Nutrition
Todd Callaway
Department of Animal and Dairy Science
Kylee Jo Duberstein
Department of Animal and Dairy Science
Qun Zhao
Department of Physics & Astronomy
Elizabeth Howerth
Department of Pathology
Holly Kinder
Department of Animal and Dairy Science
