The University of Georgia has entered into a collaborative research agreement with GeoVax Labs, Inc. to develop and test a vaccine to prevent infection from the emerging Zika virus.
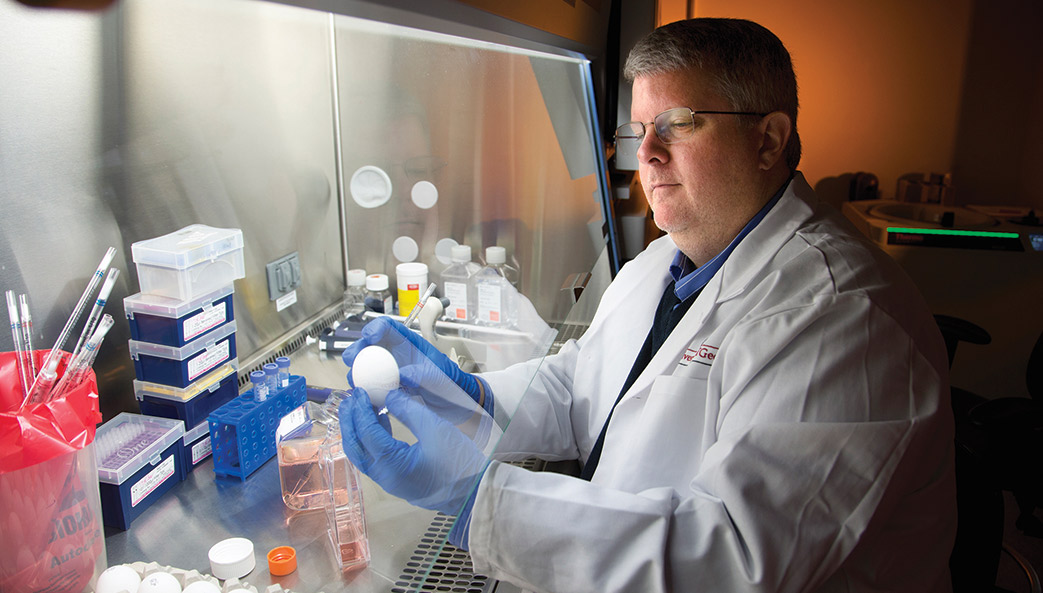
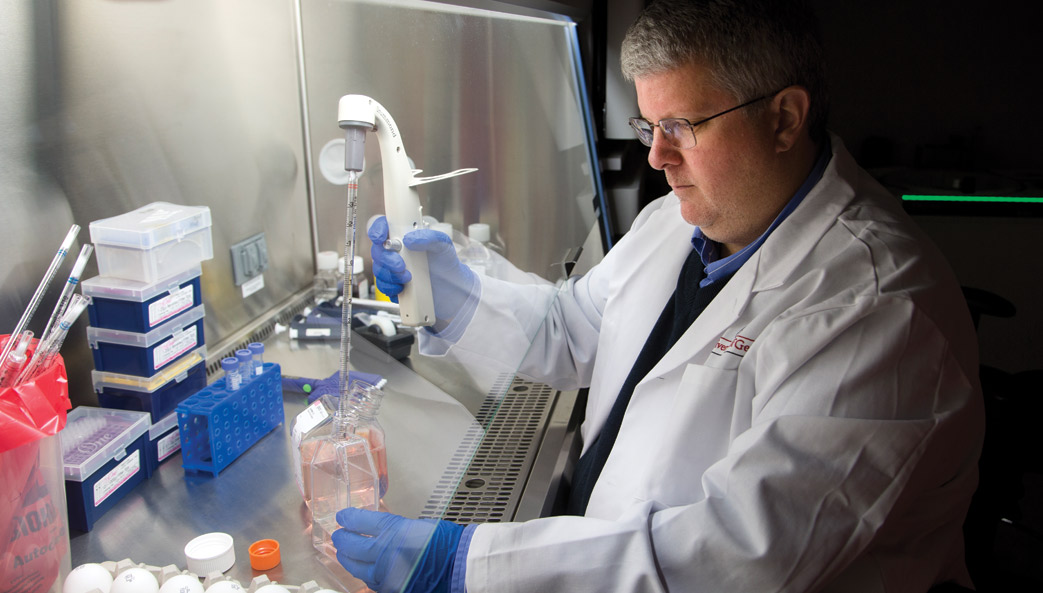
The collaboration will combine the vaccine-development expertise of UGA researchers, led by Ted Ross, director of UGA’s Center for Vaccines and Immunology, with GeoVax’s novel vaccine-platform technology. Ross, a professor and Georgia Research Alliance Eminent Scholar in Infectious Diseases at the College of Veterinary Medicine, joined UGA last fall.
The mosquito-transmitted Zika virus is linked with birth defects in thousands of babies in Brazil and elsewhere; and with Guillain- Barré syndrome, a disorder in which the body’s immune system attacks the nervous system. The virus is expected to spread to most of the Western Hemisphere, with Gulf Coast states bearing the brunt of Zika outbreaks in North America.
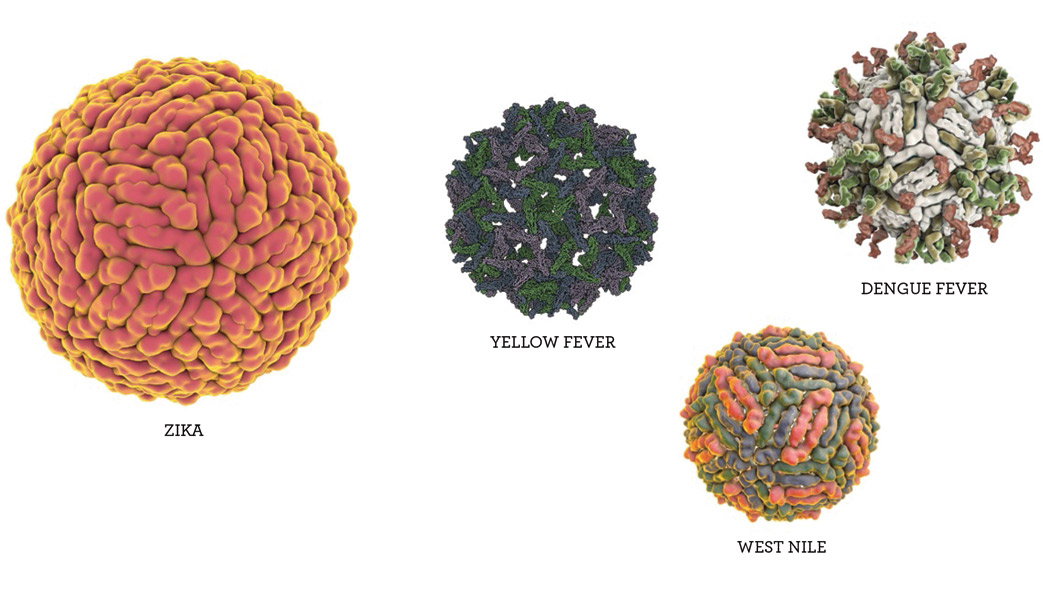
There is no proven vaccine or treatment for Zika—closely related to the yellow fever, dengue, and West Nile viruses, which also are transmitted to people by mosquitoes.
“We believe that the expertise of our researchers combined with GeoVax’s vaccine platform can accelerate the development and testing of a vaccine for this fast-spreading viral disease,” Ross said.
Ross’s research group specializes in designing, developing and testing vaccines—including what are called VLP-based vaccines—for viruses like those noted above as well as Ebola, influenza, respiratory syncytial and HIV/AIDS.
VLPs—“virus-like particles”—mimic a live virus but do not contain genetic material; although they cannot cause infection, they elicit a strong immune response in the cells of the person being vaccinated.
Ross explained that vaccines made with VLPs give the immune system a head start in preventing infection. “When a person vaccinated with a VLP is infected by the real virus,” he said, “the immune system is ready to fight back.”
Vaccines using VLPs on today’s market are used to prevent hepatitis and papillomavirus infections, and others are in development.
GeoVax’s vaccine-platform technology takes a different approach with VLPs. Instead of introducing them in the vaccine, it uses recombinant DNA or recombinant viruses to produce VLPs in the person being vaccinated. In that way, they more closely resemble the virus generated in a person’s body during a natural infection.
The Atlanta-based company’s VLP platform has so far been used in vaccines against HIV and hemorrhagic fever viruses, including Ebola, Marburg and Lassa. The HIV vaccine has been proven safe in human clinical trials involving over 500 individuals. It also is being evaluated for use in cancer vaccines. “We believe our vaccine platform is uniquely suited to apply to the Zika virus,” said Robert McNally, GeoVax president and CEO.
Ross’s lab will test Zika VLP vaccines developed by GeoVax, as well as any emanating from his own research team.
In addition to Ross, UGA researchers working on Zika vaccines will include Ralph Tripp, Georgia Research Alliance Chair in Vaccine and Therapeutic Development; Biao He, Georgia Research Alliance Distinguished Investigator; Fred C. Davison, Distinguished University Chair in Veterinary Medicine; and Mark Tompkins, associate professor of infectious diseases.
 Zika’s extended family
Zika’s extended family
Zika is actually a part of a notorious family of disease-causing pathogens called flaviviruses. Their name comes from the Latin “flavus,” which means yellow, a reference to the jaundiced skin and eyes of patients infected with yellow fever virus. Other members of the family include dengue virus, West Nile virus and Japanese encephalitis virus.
The good news about the relationships between these pathogens is that scientists have studied many of Zika’s cousins extensively, and the lessons they have learned may help speed discovery.
“Zika virus has a lot in common with other flaviviruses,” said Ross. “Vaccine candidates have been developed for dengue, West Nile and yellow fever, so that gives us encouragement that we can develop a vaccine for Zika virus as well.”
West Nile: Maintained in a natural cycle of transmission between birds and mosquitoes, West Nile virus can cause fatal neurological disease in humans, and it spread throughout much of the United States following the first reported cases in Queens, New York in 1999.
Yellow fever: Found in tropical and subtropical areas of South America and Africa, yellow fever generally only causes mild illness. However, approximately 15 percent of cases progress to a more severe form of the disease, which is characterized by high fever, jaundice, bleeding, shock and organ failure.
Dengue fever: Dengue fever is a leading cause of illness and death in tropical and subtropical regions throughout the world, infecting as many as 400 million people every year. In its most severe form, the infection causes blood vessels in the body to leak, which may lead to failure of the circulatory system.
Japanese encephalitis: While rare, fatality rates among those who develop encephalitis (an inflammation of the brain) from Japanese encephalitis virus can be as high as 30 percent. People who survive severe infections may experience permanent intellectual, behavioral or neurological problems, including seizures or paralysis.