Medical devices and implants can be life-saving, but they also open the body up to two major health concerns: biofilm and blood clots. Two University of Georgia researchers have developed a material that solves both problems.
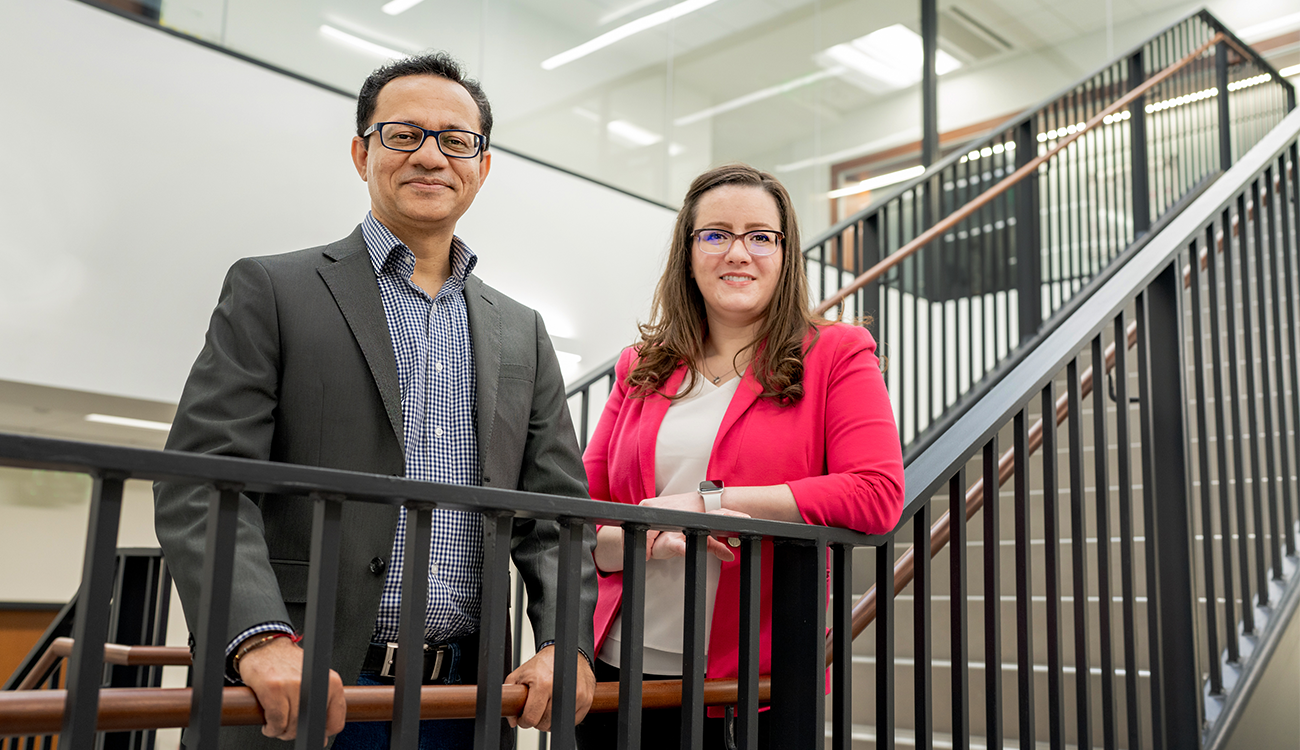
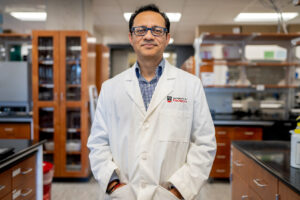
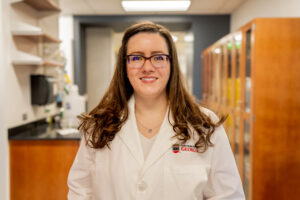
Hitesh Handa and Elizabeth Brisbois, faculty members in UGA’s College of Engineering, have found a way to improve these medical devices by using a naturally occurring gas in the body, nitric oxide. The method has been shown to drastically reduce the chances of infection and blood clotting, medical concerns that can lead to emergencies like heart attack, stroke or sepsis.
Now, by commercializing this technology through their company Nytricx, Handa and Brisbois hope to maximize its impact.
“Both Hitesh and I like doing research, but we’re both the type of people who are really driven by the application,” said Brisbois, assistant professor in the School of Chemical, Materials and Biomedical Engineering. “We want to be able to translate these technologies to the actual application in the real world.”
Establishing a partnership
This isn’t the first time Handa and Brisbois have collaborated. In fact, they have been collaborating together for several years, which has already resulted in several funded NIH R01 grants, publications and patents.
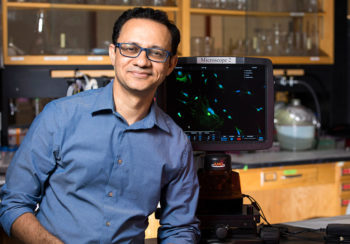
After receiving his doctorate, Handa worked in the University of Michigan’s Department of General Surgery as a research investigator under renowned surgeon Dr. Robert Bartlett. Brisbois also completed her training at the University of Michigan, earning her Ph.D. in chemistry under the guidance of Mark Meyerhoff, a renowned electrochemist and nitric oxide chemist, followed by her NIH-funded postdoctoral fellowship.
Handa joined UGA in 2015, and Brisbois joined more recently in 2020. The two have complementary skills and mutual research interests, and their partnership was born. It has led to a multidisciplinary lab that conducts translational biomaterials research aimed at bringing these technologies from benchtop to bedside.
“I knew his lab was set up really well to do a lot of the biological and animal studies for research,” Brisbois said. “So, that was a great opportunity for us to collaborate and push these challenging projects forward.”
Biofilm and blood clots
More than half a million people each year develop health care-acquired infections during stays in hospitals and nursing homes. According to the Centers for Disease Control and Prevention, approximately one in 31 U.S. hospital patients and one in 43 nursing home residents contracts at least one infection in association with their health care. These infections most commonly come from devices like catheters or ventilators, a problem exacerbated by the COVID-19 pandemic.
“Patients can get an infection when that was not even the main problem they had initially,” Handa said. “If we can make any improvement in the current materials of medical devices, we can actually help patients by avoiding these additional complications.”
So, why do these infections occur?
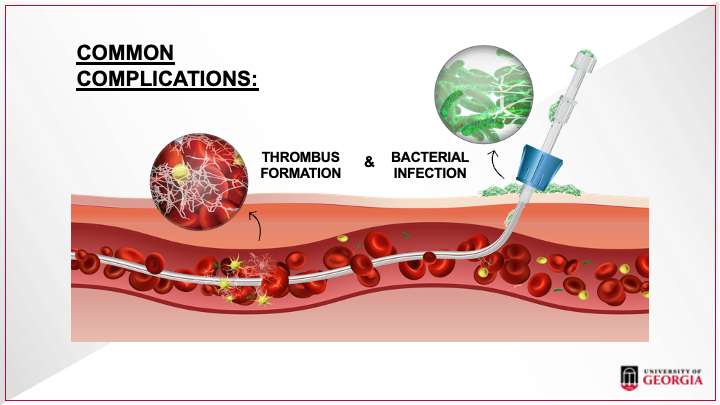
The body recognizes invasive devices like catheters as foreign entities, prompting the blood to clot as a protective mechanism. Biofilm forms when bacteria stick to the device surface and clump together, forming a layer of microorganisms. This spreads throughout the surface of the device and enters the body, leading to infection.
Most medical devices currently on the market are simply not equipped to handle both of these problems at once.
“Most available treatments address either clotting or infection, not both—and not very efficiently, because bacteria can develop resistance toward those materials” Handa said.
However, devices coated in a nitric oxide material address both concerns simultaneously.
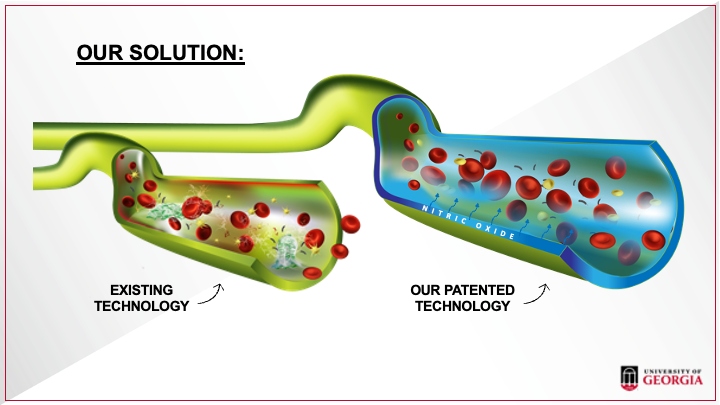
“Medical devices currently on the market cannot fight the biofilm, but nitric oxide can,” he said. “It can disperse biofilms and has multiple mechanisms to kill bacteria. It’s also very difficult for bacteria to develop resistance towards. Just by using nitric oxide, we can take care of both clotting and infection with one coating.”
Nitric oxide helps signal the blood vessels in your body to relax, allowing them to expand and blood to flow freely to every part of your body. It also sends a signal to prevent platelet activation which, then, prevents clotting. It’s why your parents forced you to stay at the dinner table until you finished your greens. When you consume foods high in nitrates, such as spinach, arugula and kale, your body turns those nitrates into nitric oxide.
“When we are making surface coatings or new materials, we are designing them in such a way that they can release nitric oxide gas just like our body does,” Handa said. “So, when they come in contact with bacteria or blood, blood won’t clot on the surface, platelets won’t get activated and the bacteria won’t infect the surface of that medical device.”
To doctors, a treated device would look just like a regular catheter or other instrument.
“But the catheter material is made with the right chemistry to produce this nitric oxide in a controlled way,” Brisbois said.
From concept to commercialization
To help move this technology closer to market, Handa has taken advantage of the resources and services UGA’s Innovation District has to offer, particularly Innovation Gateway.
Based in the Office of Research, Innovation Gateway is UGA’s go-to resource for research commercialization, helping investigators protect intellectual property and then license those technologies, either to existing companies or to their own startups (which Gateway can also help launch). It’s one of the key components of the university’s Innovation District initiative.
“When we have some data we think seems novel, we just send it to Innovation Gateway,” Handa said. “They have the expertise to guide us and file for a patent if the findings are worthy.”
One of those experts is Cory Acuff, associate director of licensing in Innovation Gateway. When Acuff and his fellow licensing managers receive an invention disclosure, they start by reviewing it in-house, looking for the potential application, novelty and market of the invention.
“Sometimes this information can be quickly identified,” Acuff said. “Other times, early-stage inventions may take a while to figure out where they could be applied in the market.”
According to Acuff, Handa is named on 26 invention disclosures. While not all of them have moved forward, that number makes him one of UGA’s most prolific inventors in the biological services and engineering technology space.
“Whenever I need help, I know I can email Gateway and ask my questions,” Handa said. “Which is great because, at my stage, you know a little bit about startups but you are not an expert. You need experts who can help you understand the complications associated with technology transfer and commercialization.”
Once an invention is disclosed and protected, researchers can choose to form their own startup company to move it closer to market. Innovation Gateway’s startup arm offers several programs to help get ideas off the ground and moving. When a UGA faculty member wants to form a startup, they come to see Ian Biggs, director of startups at Innovation Gateway.
“Most of these breakthrough technologies are proven in the lab, but industry really needs a successful demonstration of a product incorporating the technology in the environment in which it will be used before they will invest,” Biggs said. “Startups are the mechanism by which that practical demonstration can occur.”
One way to demonstrate that is through NSF I-Corps, a customer discovery program where participants identify, test and validate customer segments over an eight-week program. Additionally, they’ll learn how to create and hone a value proposition for their product or business.
After I-Corps is completed, participants are able to continue to use the coaching and mentoring services offered by Innovation Gateway to reach a final decision to move forward with their business and enter the startups pipeline.
“My training is more on the technical side of things, but being able to work with Innovation Gateway helps me understand better what it actually takes to get these new technologies commercialized,” Brisbois said. “We have several patents and a lot of them are for these material technologies that we think are getting really exciting results in the lab demonstrating their potential to overcome medical device challenges.”
Nytricx is currently moving forward with its nitric oxide research and focusing on vascular and urinary catheters, as well as vascular grafts. These products are being optimized while the researchers perform shelf life studies, antimicrobial testing and test packaging and transportation stability. Nytricx is also moving forward with studies using animal models while they continue to look for funding opportunities from grants and investors.