Researchers from the University of Georgia are part of an international investigation led by the Yale Department of Psychiatry to better understand the cause and effect of schizophrenia in some high-risk adolescents and young adults.
The research, funded by a $52 million grant from the National Institutes of Health, will fund the development of the Psychosis Risk Outcomes Network, or ProNET. The consortium will be based at 27 institutions, where investigators will characterize phenotypes associated with the clinical high risk or prodrome state of schizophrenia in adolescents and young adults.
The study is the largest multisite collaborative psychosis risk study conducted in the world to date.
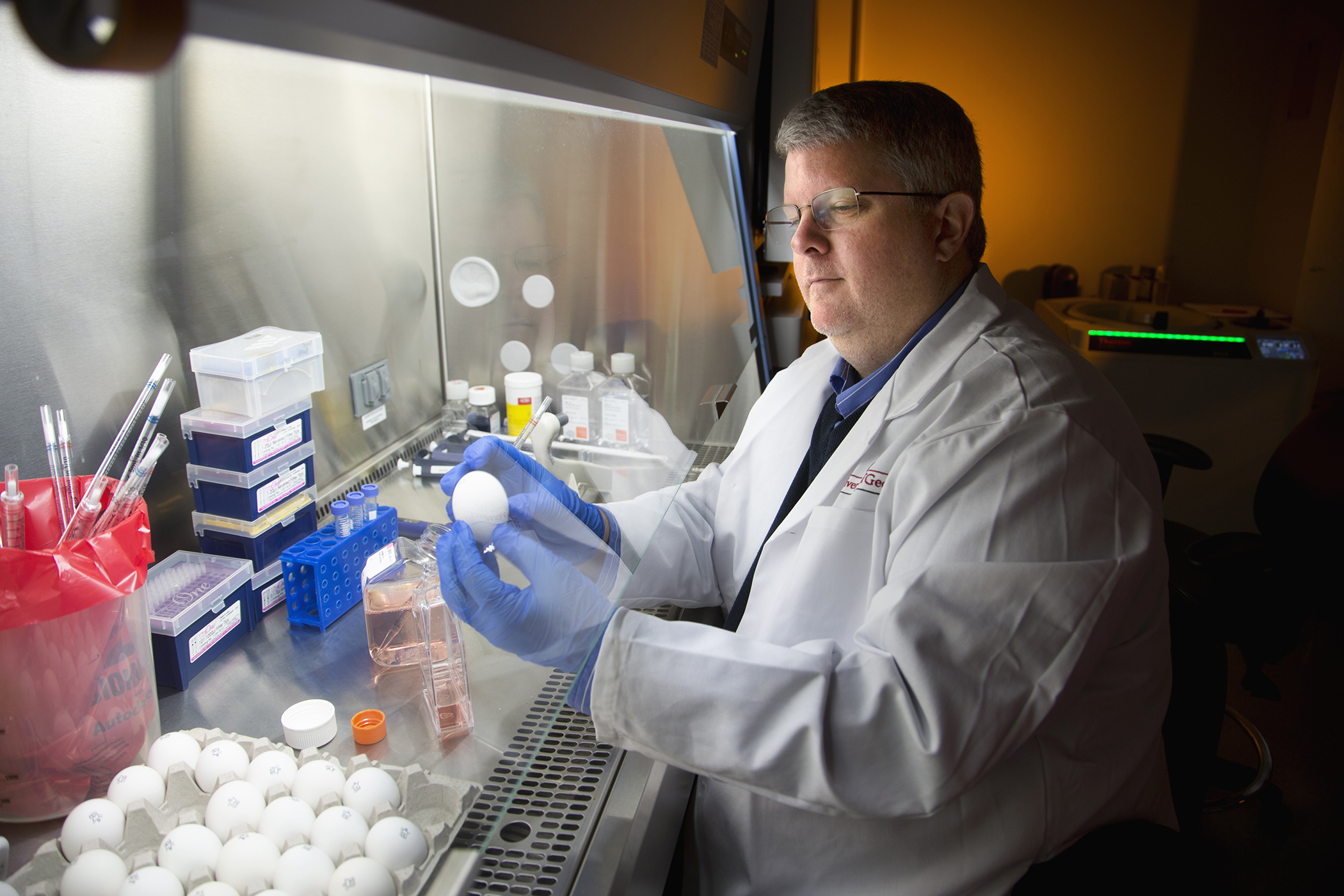
Gregory Strauss, assistant professor of psychology in the Franklin College of Arts and Sciences, is a site PI on the grant, which is being used to establish the ProNet consortium. ProNet was developed to allow the field to rapidly test hypotheses about biomarkers leading to the development of psychotic disorders (e.g., schizophrenia) and to build the infrastructure for multinational clinical trials using a personalized medicine approach.
Across all 27 sites, the investigators will recruit 1,040 patients at clinical high-risk for psychosis and follow them for two years. Strauss and his UGA team of collaborators will collect a series of measures on the participants, including clinical interviews, neuropsychological tests, MRI measures of brain structure and function, EEG, blood and salivary fluid biomarkers, genetics, natural language, and mobile phone digital phenotyping.
“Psychotic disorders are one of the leading medical causes of functional disability worldwide,” Strauss said. “Given that most individuals do not recover after the onset of a psychotic disorder such as schizophrenia, the field has been shifting toward a model of early identification and prevention in those at clinical high risk for developing psychosis.”
Strauss’ role is to lead data collection efforts at UGA, as well as clinical portions of the grant focused on his specialty—negative symptoms (reductions in motivation, emotion, social behavior). He is also a key contributor to the consortium’s efforts related to digital phenotyping and mobile assessment of symptoms and behavior.
“Psychotic disorders are often proceeded by a prodromal, or pre-illness, period where subtle symptoms arise and functioning deteriorates two-four years before the illness onsets,” he said.
ProNet will help to address these problems facing early identification by developing novel risk prediction algorithms based on combinations of biomarkers, clinical variables, cognitive tests, genetics and digital phenotypes. The algorithms are critical for identifying mechanistic targets needed to guide drug development and creation of personalized treatment approaches to prevention and early intervention.
Psychosis is a very heterogeneous disorder, with multiple syndromes or pathways in its constellation of symptom combinations. Multiple treatments will therefore be necessary to slow or prevent its onset in those at clinical high risk for developing it.
Strauss’ lab at UGA is one of 27 sites, including 18 in the United States, two in Canada (Calgary, McGill), two in the United Kingdom (Cambridge, Kings College), and single sites in Italy (Pavia), Spain (Hospital Grego), Germany (Munchen), China (Shanghai Medical Center), and South Korea (Seoul National University).
The grant is a component of NIH’s launch of a new public-private partnership to meet the urgent need for early therapeutic interventions for people at risk of developing schizophrenia. Part of the Accelerating Medicines Partnership, AMP Schizophrenia brings together NIH, the U.S. Food and Drug Administration and multiple nonprofit and private organizations.
These partners will work toward the shared mission of discovering promising biological markers that can help identify those at risk of developing schizophrenia as early as possible, track the progression of symptoms and other outcomes and define targets for treatment development.
“We know that with most brain diseases, early interventions before the onset of symptoms improve long-term outcomes,” said NIH Director Francis S. Collins. “Through research we’ve identified clinical and biological markers for schizophrenia, but we need to translate this knowledge into early interventions to make a meaningful difference in the lives of people at risk for this debilitating disease. AMP Schizophrenia aims to be that bridge.”
This research is supported by the National Institute of Mental Health of the National Institutes of Health under award number U01MH124639. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.