 Stephen Dalton is director of the Center for Molecular Medicine (CMM), founded in 2012 with a focus on translational research—taking basic research findings and converting them into therapies for human diseases, cures and diagnostics. The center moved this fall into a new $25 million, 43,000-square-foot-facility that will house newly hired faculty and up to 10 research groups. Dalton, professor and Georgia Research Alliance Eminent Scholar of Molecular Cell Biology, discusses the importance of translational research, the state of stem cell research and the biggest problem faced by scientists.
Stephen Dalton is director of the Center for Molecular Medicine (CMM), founded in 2012 with a focus on translational research—taking basic research findings and converting them into therapies for human diseases, cures and diagnostics. The center moved this fall into a new $25 million, 43,000-square-foot-facility that will house newly hired faculty and up to 10 research groups. Dalton, professor and Georgia Research Alliance Eminent Scholar of Molecular Cell Biology, discusses the importance of translational research, the state of stem cell research and the biggest problem faced by scientists.
What is molecular medicine?
Molecular medicine is quite a broad topic, but what it really means is taking our understanding of cell structure and cell function at the molecular level, and using that information to try and generate new therapies, which themselves are often molecular. It’s really a reflection of both the molecular level of research that’s being done, but also the therapeutic solutions that will arise from the research—new medicines, new drugs, new vaccines. Every researcher in the center will have a direct interest in curing and understanding at least one type of disease, whether that be neurological, such as Parkinson’s and Alzheimer’s and dementia, or cardiovascular, such as heart disease and stroke, or metabolic, such as diabetes.
What do you find appealing about translational research?
I think doing basic research is intellectually stimulating, but I think that at the back of everyone’s mind is making an impact on society and supporting UGA’s broader mission, which is to help the community and to provide solutions. I think that’s important. We can’t just ask intellectually interesting questions for the sake of it—there has to be an endpoint and some utility and value for the community. The way that I like to see science working is for researchers to do great, cutting-edge basic science, but then take the findings of those experiments and apply them for the greater good.
Will CMM researchers be working with stem cells?
That’s going to be an important part of it, but it’s not the only iron in the fire. You need to use multiple research models to really understand complex biological questions and then develop therapies and cures. You need to use animals to understand disease progression, so there are going to be mouse models. We’ll also be doing things like drug screens—looking for new drugs that can help cure diseases. And we’ll be developing new diagnostic techniques to help us better understand diseases and develop therapies.
Last year marked the 10th anniversary of the discovery of induced pluripotent stem (iPS) cells. What kind of impact has that had?
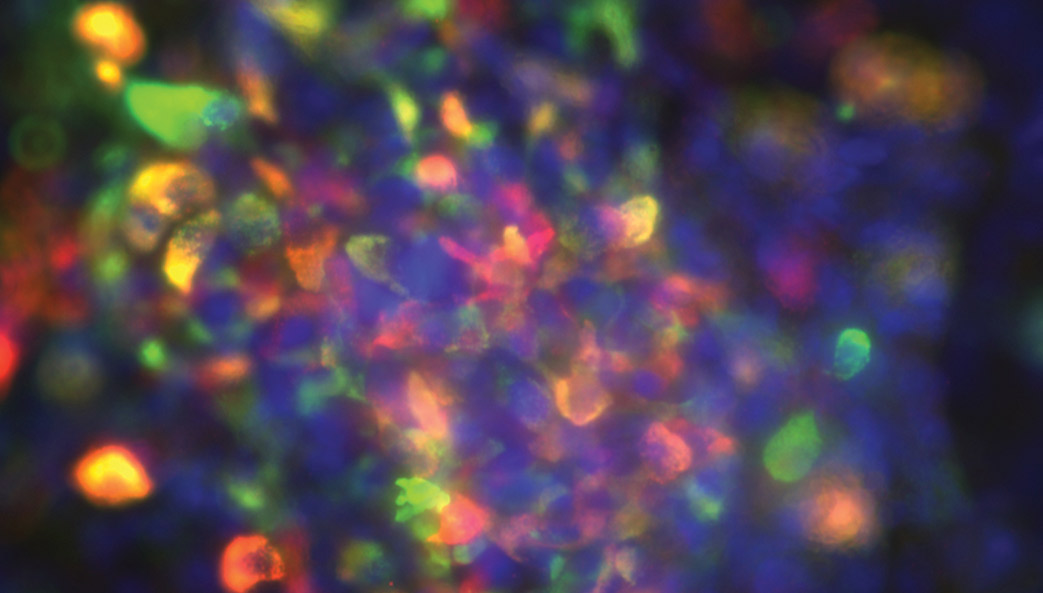
The introduction of iPS cells—cells that are generated directly from adult cells—has really transformed the stem cell field in many ways. It’s removed the ethical problem of working with pluripotent cells—undifferentiated cells that have the ability to differentiate into specialized cells—because previously they were derived from embryos.
There are a number of different ways that you can use iPS cells and pluripotent cells for drug screening and therapies. One is for transplantation into a patient. There are some clinical trials underway where you can take iPS pancreatic cells and transplant them into people with type 1 diabetes, where they produce insulin and help control glucose levels in the bloodstream. That’s very promising. There are also trials for using iPS cells to treat macular degeneration and Parkinson’s disease. I expect there will be more and more such applications over the next five to 10 years. There’ll also be therapies designed for a number of blood disorders, such as sickle cell disease.
However, I think the biggest impact these stem cell models will have is in drug discovery for the development of new therapeutics, as they provide a plentiful source of patient-derived cells to screen or test experimental drugs. I expect that it will have a massive impact over the next decade.
What challenges do you anticipate during the center’s first decade?
The big problem that all researchers face now, and probably for the next 10 years, is the tightness of the budgets coming from the federal government, whether it be the National Institutes of Health or the National Science Foundation. Budget lines are a real concern because that’s the lifeblood of research—getting the funding to hire graduate students, postdoctoral fellows and technicians to push the program forward. Fortunately, the people we’re hiring are really top notch, and we anticipate they’re going to be competitive. But it is always a worry when you hear less-than-positive things about funding levels.