Globally, efforts to control malaria caused by Plasmodium vivax are lagging behind that of other species of Plasmodium due to its unique biology. A team of researchers at the University of Georgia, the Institute Pasteur of Cambodia, and Shoklo Malaria Research Unit in Thailand detail a new screening tool and report for the first time a method capable of discovering novel experimental drug compounds for use against vivax malaria. Their study was recently published in Scientific Reports.
The parasite species P. vivax is the most widespread cause of malaria. While not as deadly as malaria caused by P. falciparum, it can cause severe disease and has a significant impact on both national economies and personal finances, in part due to this species’ propensity to cause relapses.
Relapses are caused by hypnozoites, a form of the parasite residing in the liver, which can lie dormant for a period of time before causing another symptomatic blood infection. During this period of dormancy, hypnozoites are not susceptible to standard antimalarials, meaning a patient treated for a blood infection is not fully cured.
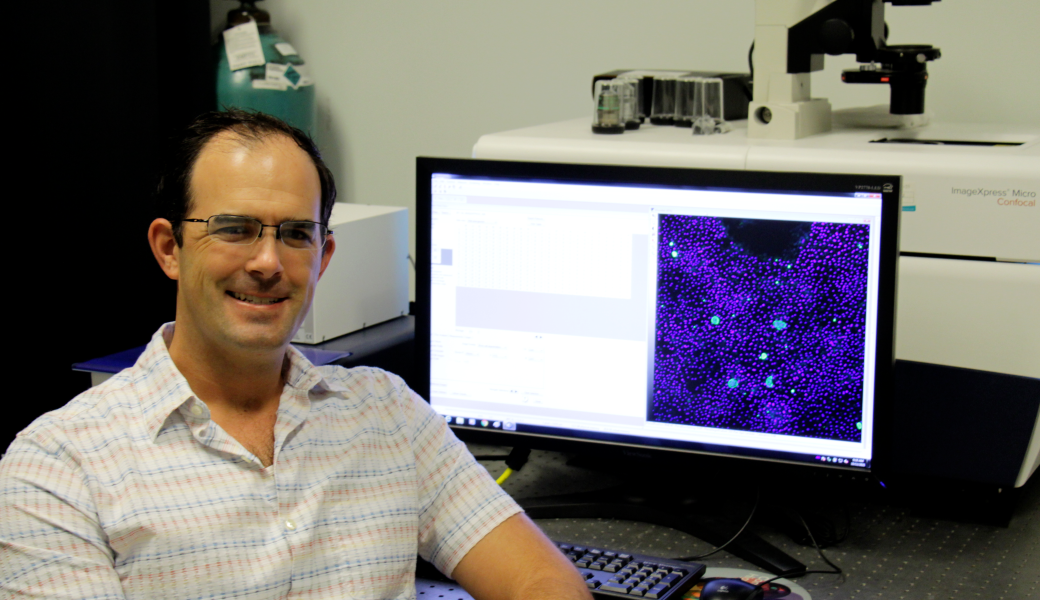
“With this assay, we can now tell earlier on in the drug discovery process if a compound is going to work against hypnozoites,” said Steven Maher, assistant research scientist at the Center for Tropical and Emerging Global Diseases and lead researcher on the study. “In this study, we were able to identify three new drugs that kill dormant hypnozoites.”
One of the drugs identified looks promising as a possible new treatment, though Maher said it will need more testing. The other two could be useful in studying hypnozoite biology and increase understanding of such things as the mechanisms of dormancy.
The team’s report also shows how two current antimalarial drugs, chloroquine and tafenoquine, synergistically work together to kill hypnozoites. However, these drugs cannot be administered to children and pregnant women (due to their known side effects), nor to people who lack the enzyme called G6PD. Up to 20% of the population in southeast Asia are G6PD deficient.
“The current drug therapies work well to treat the symptomatic blood stage of vivax malaria,” said Steven Maher. “However, in vivax malaria we need to eliminate hypnozoites to fully cure the patient, and for that we need new therapies.”
To compound the problem, typical mouse models used in malaria drug research can’t determine if the experimental compounds work against hypnozoites because the Plasmodium species that infects mice doesn’t produce them. Additionally, because the assays used as the first step in discovering potential new drug compounds focus on the blood stage of the parasite, researchers need a different kind of assay that will allow them to test these compounds on hypnozoites, which requires a stable culture of liver cells.
“It’s a challenge because you have to get samples from where the vivax malaria is endemic,” said Maher. “Liver cells don’t stay viable in culture for long, and these assays take eight days to show results. The assay itself is difficult to run, but we have a great team of researchers in Cambodia and Thailand that has really helped to make this possible.”
The team is continuing to build better tools to overcome the challenges drug discovery in P. vivax faces as they begin to test these drugs in animal models.