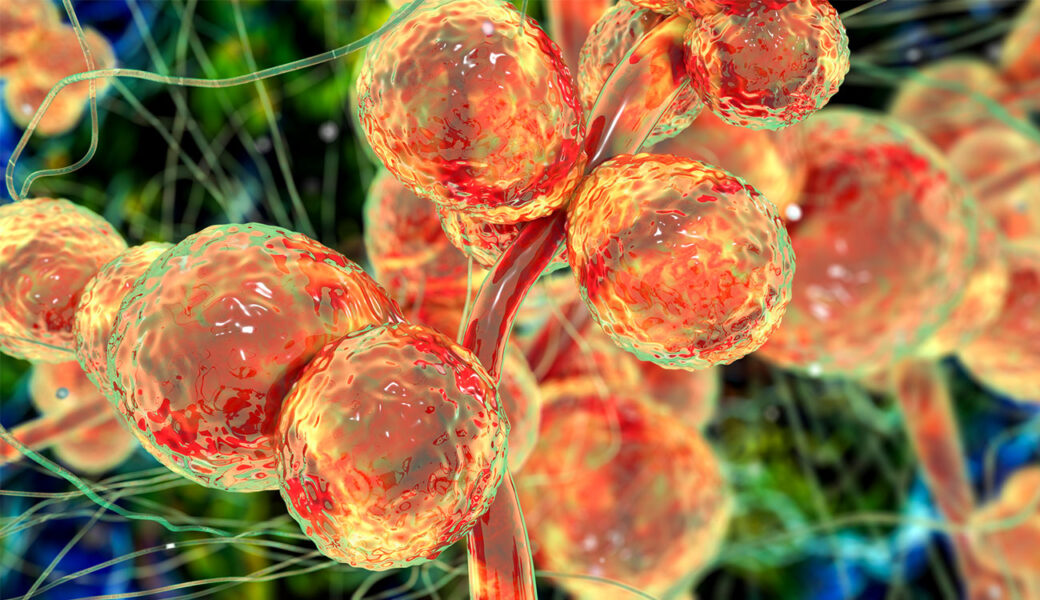
It starts out with a cough and slightly slurred speech. Then come the muscle spasms and dramatic mood shifts.
In HBO’s hit show “The Last of Us,” these are the beginning signs that a human has contracted a fungal infection that turns people into zombies and rips through the fabric of modern society.
The premise may sound improbable, but it is based on a very real fungus that really does infect brains and bodies, turning its victims into mindless, zombie-like creatures.
Ophiocordyceps unilateralis, known as Cordyceps, is a parasitic fungus that infects insects like ants through spores and uses its new host to infect other insects in the vicinity.
While this fungus is not a threat to humans because of our higher internal body temperatures, others can be serious. Last October, the World Health Organization flagged a list of fungal pathogens that were public health threats, stressing the need to prioritize research and development that strengthens the global response.
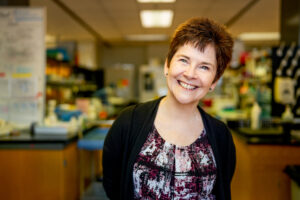
“There are at least 1.5 million deaths a year caused by invasive fungal infections,” said Michelle Momany, professor of plant biology in the Franklin College of Arts & Sciences. “But people don’t think about fungal diseases as a serious threat to human lives and public health.”
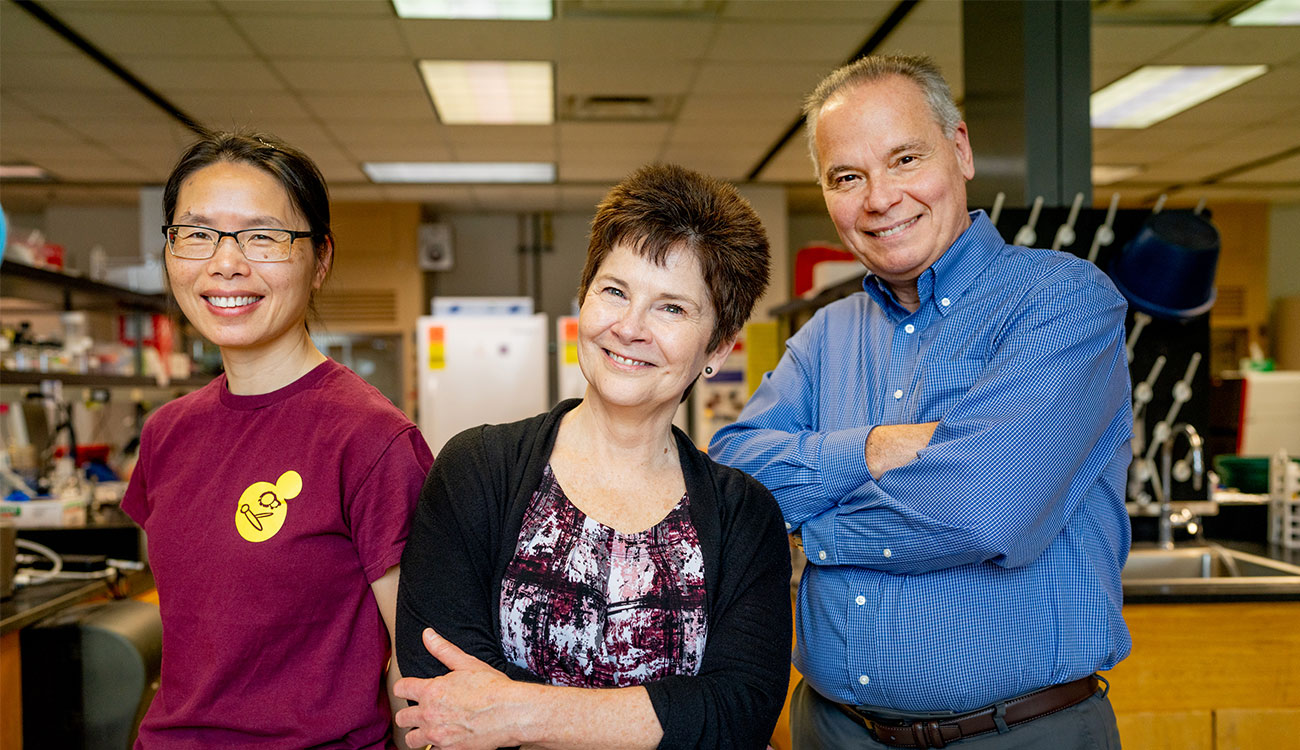
UGA has become an international leader in fungal research thanks to its interdisciplinary Fungal Biology Group, where researchers focus on better understanding the biology of fungi and the threats fungal pathogens pose to humans and plants.
Aaron Mitchell, professor and head of Franklin’s Department of Microbiology, said he was always the “token fungi guy” at an institution—until he joined UGA.
“There’s a real community of researchers here working in mycology,” he said. “We have created an open forum to discuss research, and when you want to explore something outside of your specific expertise all you need to do is walk down the hallway to see if someone else has the right technology or can offer the insights you need.”
Over a dozen researchers at UGA conduct groundbreaking science in this understudied but critical field.
The Big Four pathogens
Unlike the zombie insect fungus, the major fungal pathogens that pose the greatest risk to humans can survive the heat of the human body.
“One of the biggest factors that determines whether a fungus will be a threat to humans is whether it has the ability to grow at a human body temperature of 37 degrees Celsius,” Mitchell said. “Most fungi aren’t capable of surviving in that heat, so they can’t mount an infection.
“But the few that can do the dirty work of infecting humans.”
These include Cryptococcus neoformans, Aspergillus fumigatus, Candida albicans and Candida auris. They are known as opportunistic pathogens because they’re prevalent in the environment and human bodies, and are not usually a problem for human health. But that can change if someone’s immune system is compromised, opening a window for an infection to strike. The most vulnerable groups are people with AIDS, cancer, diabetes or other autoimmune diseases, or who have had organ transplants or implanted medical devices.
“All signs are pointing to the fact that the disease burden from fungal pathogens will only increase,” Mitchell said. “And that’s because the at-risk population is increasing in size.”
Mitchell specializes in C. albicans and C. glabrata, two leading pathogens that cause over 10,000 deaths annually in the U.S. and more than 400,000 worldwide. They’re also part of every human’s microbial makeup, living in our bodies mostly without issue.
“There’s a real community of researchers here working in mycology. We have created an open forum to discuss research, and when you want to explore something outside of your specific expertise all you need to do is walk down the hallway to see if someone else has the right technology or can offer the insights you need.”
– Aaron Mitchell, professor and head of Franklin’s Department of Microbiology
When someone gets a medical device implanted—a catheter or an artificial heart valve, for example—the fungal organisms can infect tissues through the device. Because these organisms are a normal part of human biology, they are also difficult to diagnose. Their presence usually doesn’t merit alarm.
Momany focuses on A. fumigatus, a common fungus that can be found in places like compost piles and leaf litter. Most humans inhale dozens of A. fumigatus spores every day without issue. But if someone has a compromised immune system, the fungus can enter the lungs and spread to other organs, including the brain and kidneys, through fungal fibers. It currently claims around 400,000 lives a year and is especially fatal for bone marrow and organ transplant patients.
Xiaorong Lin, Gene E. Michaels Distinguished Professor in Medical Mycology, studies A. fumigatus and C. neoformans, an airborne fungus found mostly in soil, especially any contaminated with bird droppings. While it can remain dormant for decades inside the lungs of most humans, it can become severe for AIDS or organ transplant patients, as well as people dealing with certain cancer therapies or genetic disorders. Resembling a tuberculosis infection, it infects the central nervous system and brain. It claims hundreds of thousands of lives annually and is responsible for 15% of deaths in AIDS patients.
“Most people don’t even know the name of this pathogen, and it’s killing many AIDS patients,” Lin said.
Fungal infections remain challenging because they’re difficult to diagnose, often avoiding detection until an autopsy is performed. There’s also a lack of awareness about these pathogens in the medical community, meaning they’re not always on a physician’s radar when they’re examining a patient.
Even if they could be more easily detected, fungal infections are still incredibly challenging to treat, cure and prevent.
The challenge with treating fungal infections
To illustrate the difficulty of treating or eradicating fungi, Lin points to other common conditions like athlete’s foot, dandruff and mold.
“There is no cure for athlete’s foot,” Lin said. “You can try and control it but relapse is common, and it can take months of a highly toxic antifungal treatment to clear it—and that’s all for a superficial surface infection.”
Mold in a house caused by fungi is a similar situation. It is notoriously difficult to remove and requires heavy-duty cleaning products to make any progress. Now imagine that infection is worse—and growing inside your body. It wouldn’t make sense to prescribe doses of toxic bleach to treat a fungal infection.
“It’s very difficult to target a fungal infection without also damaging the host,” Lin said.
Likewise, parts of fungal biology also overlap with humans, making it difficult to target internal infections without also attacking the human body.
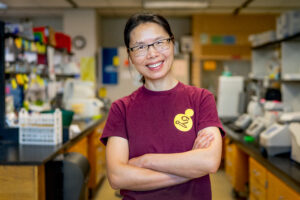
“Fungi are more comparable to cancer than a bacterial infection because, at the cellular and biochemical level, fungi are actually more similar to humans than to bacteria or plants,” Lin said. “While fungi are not actually part of us, they operate like they are.”
The first line of defense against many fungal infections is an antifungal treatment using azoles, but some fungi have also developed resistance to these antifungal medications. This development is fueled by widespread use of agricultural compounds that fight fungal disease in crops, according to research from Momany and Marin Brewer, a professor of plant pathology in the College of Agricultural and Environmental Sciences.
Momany and Brewer found that agricultural azole fungicides, which have been increasingly used to address crop loss from plant fungal diseases, are causing fungi to develop resistance to clinical azole antifungal drugs. After sampling soil, plant material and compost from agricultural sites treated with a mix of fungicides, they found fungal strains used in both agriculture and medicine that were resistant to azoles. When they looked closely at data from A. fumigatusstrains isolated from patients, they found some of them were also resistant to both agricultural and clinical azoles.
“It’s very clear that some of the issues we’re seeing in the clinic are coming from agriculture,” Momany said.
Working toward a solution
C. neoformans infects the brain, which makes it especially challenging to target with antifungal drugs. The brain safeguards itself from foreign molecules with even more intensity than other organs.
“It’s an additional barrier beyond the challenge of targeting fungal infections,” Lin said.
Lin is working in collaboration with the labs of Zachary Lewis (microbiology), as well as Richard Meagher and Suresh Ambati (both genetics), to develop a drug delivery system that can conceal the antifungal drug with a protective lipid bilayer. It’s also equipped with a special receptor protein that can recognize fungal wall molecules so it can deliver the drug to the appropriate fungal target without harming the human body.
“It’s kind of like a powerful missile wrapped in a gift bag wired to open when it detects a fungal agent,” Lin said.
They’ve tested this system on animal models and have gotten promising results against A. fumigatus and candidiasis, an infection that can caused by multiple Candida species. Based on their current data, the efficacy of the targeted drug is more than tenfold that of the untargeted drug, promising results that suggest this could be a viable option for treating fungal infections. They are currently working on testing other fungal diseases in animal models.
One of the most valuable characteristics of the innovation is that it’s a drug delivery system, so it has uses beyond treating a single fungal infection.
“This could be a really effective way to increase the potency of other drugs, as well,” Lin said.
While there are some antifungal medications, there is no vaccine against fungal pathogens. Fungal infections are as hard to prevent as they are to treat and cure because of a key difference with viral infections.
When scientists develop a vaccine for a viral infection, it’s generally apparent which protein it needs to target in order to be effective. There are limited options and it’s simpler to determine what’s causing the viral infection. In the case of COVID-19, for example, scientists quickly determined they needed to target its spike protein.
But fungal cells have around 7,000-10,000 protein coding genes, which means picking a protein to target is more complicated.
Karen Norris, a Georgia Research Alliance Eminent Scholar in the College of Veterinary Medicine, is making major headway on a vaccine to protect people against the three most common fungal infections, which are responsible for 80% of deaths.
Norris has developed an experimental vaccine and just published a new study in collaboration with Momany and other UGA researchers outlining its efficacy.
“We found there was a strong response to this vaccine with broad, cross-protective antifungal immunity in animal models,” Norris said. “Because it targets three different pathogens, the vaccine has the potential to be groundbreaking.
“One reason a vaccine approach is a challenge for these organisms is because the same populations that are at very high risk for these infections are at risk for multiple ones. A vaccine that just targets one organism is not going to be sufficient.”
So, when developing a target for the vaccine, she looked for a protein that was common in all three infections and found one that responded in all three models.
The next step is to continue collecting data to develop the vaccine for a Phase I human safety trial. Norris is excited about the potential to save lives and reduce health costs, which totals around $6 billion per year in the U.S. for fungal infections.