Doctors should be clear about the potential harms of lung cancer screenings with their patients. That is the suggestion of a recent study appearing in JAMA Internal Medicine.
University of Georgia epidemiologist Mark Ebell authored the study with colleague Kenneth Lin from Georgetown University.
Lung cancer screening is fairly new. The U.S. Preventive Services Task Force released its recommendation for lung cancer screening five years ago based on the success of the 2011 National Lung Screening Trial. However, there have been increasing concerns that screenings are producing too many overdiagnosed cases.
Overdiagnosis, says Ebell, in an underappreciated harm of cancer screening.
“What it means is that some cancers that are detected by screening never would have harmed the patient,” he said. “We’re developing technologies that are getting so good at seeing little, tiny things that even though they look like cancer, they would grow slowly enough that something else would kill the patient.”
Ebell studies clinical decision-making at UGA’s College of Public Health, and he served on the Task Force from 2012 to 2015.
The authors reviewed a collection of studies trying to determine the overdiagnosis rate of lung cancer screening, and they found that overdiagnosis is going on roughly 20 percent of the time.
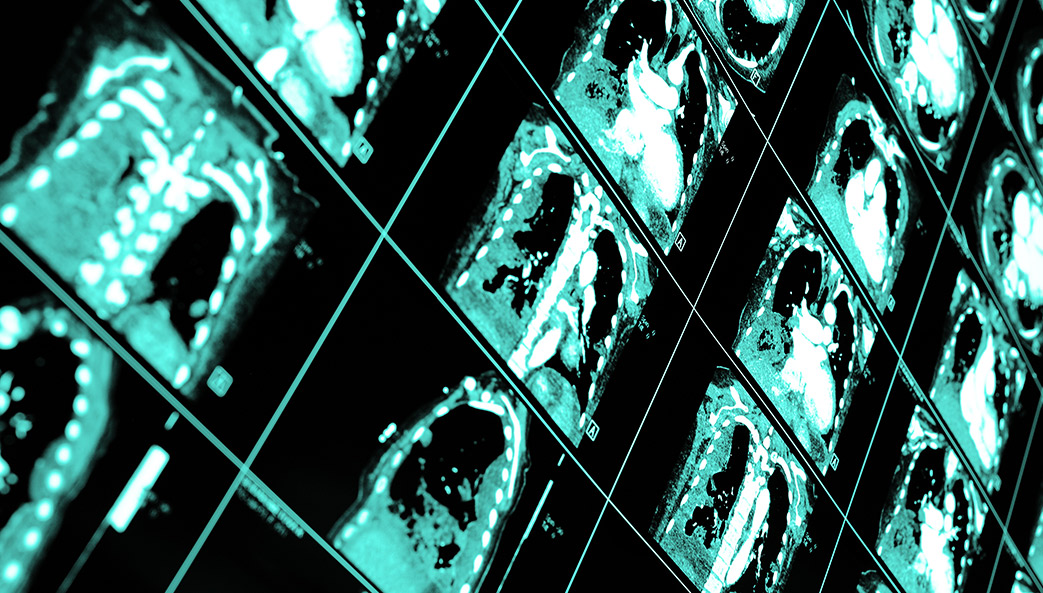
It’s important to know how often overdiagnosis occurs, says Ebell, because screenings are not without harm. CT scans expose the patient to radiation. If a lesion is found, the patient undergoes a biopsy, which is an invasive surgery.
There’s also the worry associated with any cancer screening, and of course, cost. Depending on the provider, CT scans can cost up to $10,000.
The current Task Force recommendation is to screen smokers aged 55 to 80, but recent research has revealed that older patients may not benefit from screening.
“You have to be likely to live at least another five to ten years to benefit from screening at all because what we’re trying to do with lung cancer screening is detect a very early cancer, and it takes time for that cancer to get to the point where it’s causing symptoms,” said Ebell.
The Task Force also recommends that healthcare professionals present their patients with all the available information about lung cancer screening so they can make an informed decision about whether to get screened.
Moving forward, says Ebell, more research is needed to refine the estimates of overdiagnosis so that doctors can have the most effective conversations with their patients about screening risks as they can.