Can the brain heal itself after a traumatic injury? Mesenchymal stem cells (MSCs) represent a promising treatment that could help the brain self-repair, and University of Georgia researchers have received a $3.7 million award from the National Institute of Neurological Disorders and Stroke to study MSCs’ potential for treatment of traumatic brain injury (TBI).
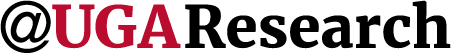
MSCs support the immune system, help nerve growth, improve blood flow, and mend tissue by releasing tiny particles called extracellular vesicles (EVs). A collaborative team from the UGA Regenerative Bioscience Center (RBC)—including Steven Stice, RBC director and GRA Eminent Scholar in Regenerative Medicine; Franklin West, professor of animal and dairy science in the College of Agricultural and Environmental Sciences; and Jarrod Call, professor of pharmacology in the College of Veterinary Medicine—will investigate their use as a treatment for TBI.
The challenge
Scientists do not fully understand how MSC-EVs affect the brain’s immune cells after TBI. “Priming,” or exposing MSC-EVs to specific conditions, could make them more effective at healing or reducing inflammation, but this process also is unclear.
In an inflammatory environment, MSCs become more active or “primed” to help regulate the immune response and minimize further damage. If the response becomes excessive and uncontrolled, it can lead to chronic inflammation, which can worsen brain damage and impair recovery.
“You really need something that can make a therapeutic impact on both protecting the brain and reducing inflammation, and possibly even helping with tissue regeneration,” West said. “Having something that can be broadly applicable across all TBIs is really important, and that’s not available today.”
The RBC team aims to create a novel framework for targeting the brain’s immune system, characterized by two key ideas: First, to study how mitochondria, the cell’s energy producers, affect brain immune cells in TBI models, looking at how energy transfer changes microglia behavior and function after injury. The second idea is to explore how priming manufacturing conditions alter EVs and their ability to control the immune response and where they travel in the body.
“We know how extracellular vesicles carry important factors and show results in treating TBI and stroke, but we don’t fully understand how they work yet,” Call said. “This research will focus on how mitochondria might be transferred through exosomes, which could answer key questions about their role in treating brain injury.”
The RBC team will create detailed profiles of various cell types involved in TBI, revealing how microglia control immune responses. They also will use experimental data and TBI models to develop quick tests that evaluate the effectiveness of extracellular vesicles. By linking lab tests with real-world TBI models, they can better choose the right conditions in which the EVs are made and ultimately improve their therapeutic potential.
The impact
The real-world impact of the RBC collaborative research is significant. According to the Brain Injury Association of America, about 2.8 million people sustain a TBI annually. Every year, approximately 64,000 people die from TBI-related injuries in the United States, which averages to about 176 deaths per day. Some estimates have put the overall economic cost of TBI injury each year at more than $75 billion.
By creating quick tests to evaluate EVs, it will speed up the development of EV therapies for TBI and possibly other neurodegenerative diseases. Identifying patient-specific cell types and tailoring EV manufacturing also could lead to more effective and personalized treatments for individuals with specific needs or conditions.
Discovering better treatments for TBI could help improve care for neurodegenerative diseases, leading to a better quality of life and slower disease progression for both patients and veterans. The Defense and Veterans Brain Injury Center reported more than 400,000 service members worldwide sustained TBI between 2000 and late 2019.
“There is still a lot we don’t know about how stem cells and extracellular vesicles work. That lack of understanding often keeps big pharmaceutical companies from stepping in to help universities or small companies develop these therapies,” said Stice. “But if we can figure out the mechanism behind how they work, it could open up more doors to get the resources we need for clinical trials. That’s the real game-changer here.”