It was just a small, angry bump when it first showed up on Don Mullis’ hand.
He’d been doing yard work and felt a pinch when he reached into a box where he stores gas cans. He must have been bitten by one of the spiders living near the box.
 “Didn’t think much about it,” he said. “Went in and did my first aid on it.” But then the spider bite got infected. “It was eating the flesh away from my body—that’s when I got concerned.”
“Didn’t think much about it,” he said. “Went in and did my first aid on it.” But then the spider bite got infected. “It was eating the flesh away from my body—that’s when I got concerned.”
He headed to the doctor, where the wound was swabbed and sent to the lab to see what he was dealing with. It was MRSA, one of the most well-known “superbugs” (bacteria that have become highly resistant to the antibiotics meant to kill them), and one that is often mistaken for a spider bite at first. It’s also potentially life threatening if it spreads inside the body.
Mullis was in for a long ride.
Desperate Times
Fighting antibiotic resistance is a never-ending struggle. By the time a new antibiotic is tested and proven effective, the bacteria it’s meant to fight are often already developing resistance to it.
The World Health Organization calls antibiotic resistance “one of the biggest threats to global health, food security and development” in the modern world. Superbugs like MRSA are predicted to kill 10 million people worldwide by 2050—more than cancer, traffic accidents, measles, cholera and tetanus combined.
“We’ve gotten to the point now where people are dying from a urinary tract infection, which is something our parents would have never thought possible,” said Stephen Trent, an infectious diseases professor at the University of Georgia. He’s even seen physicians on Twitter pleading for some new and effective treatment to stop a patient’s raging antibiotic-resistant infection. Sometimes, they’re forced to employ specialized viruses that can kill the bacteria.
“That’s how desperate we are,” Trent says. “Because no antibiotics work, patients are just going home and dying. Diabetic foot patients are going home sometimes with a pad with maggots in the bottom of it to eat the bacteria in the heel of their feet because we can’t cure the infection with antibiotics anymore.”
To combat the infection in Mullis’ hand, doctors tried several combinations of antibiotics before settling on one that he would have to take for a year.
The doctor told him they were going to saturate his body with medication in an effort to kill the bacteria.
The last 81 years flashed through Mullis’ mind.
One Step Forward, Two Steps Back
One of the main focuses of Trent’s lab is how bacteria become resistant to colistin, a last resort antibiotic used to fight bacteria when nothing else will work. “We don’t like to use it because it can shut down your kidneys and cause kidney damage, but we’ve gotten to the point where we don’t have a choice,” he says. Like with other antibiotics, though, bacteria have now become resistant to colistin as well.
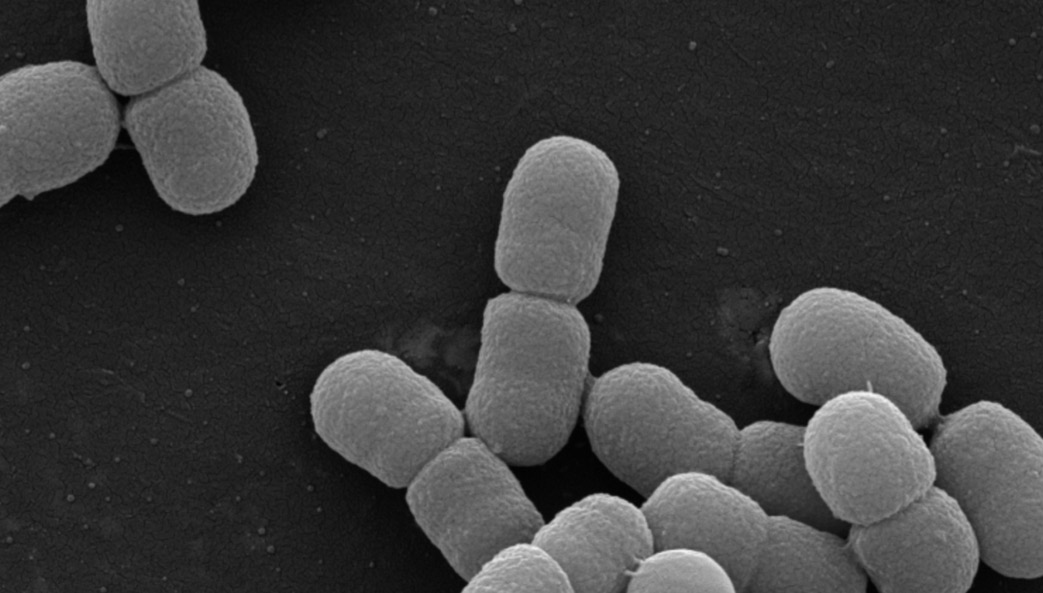
His lab concentrates on discovering how bacteria become resistant to colistin and looks for compounds (combinations of antibiotics) that can make the bacteria vulnerable to the disease-killing drug again. Trent’s work has led to a broader understanding of how bacteria change their surface, which he likens to armor, to fight off antibiotics and has been funded by the National Institutes of Health since 2002.
His lab also works on vaccine development, which at first seems like a completely separate arena but is actually very connected to the issue of antibiotic resistance. Better vaccines mean stopping bacterial infections before they can start.
In 2013, while at the University of Texas-Austin, Trent developed a technology to produce new adjuvants, substances in vaccines that increase the body’s immune response. He genetically engineered more than 60 strains of E. coli to make new adjuvants for vaccine production.
More recently, Trent and his UGA colleagues received a $3.2 million grant from the National Institutes of Health to develop a vaccine platform that engineers the surface of a bacterium to serve as the vaccine. The platform, called SAAVE (Surface Antigen/Adjuvant Vaccine Engineering), would allow it to be taken orally. For a vaccine to pass the World Health Organization’s standards, it has to be cost effective, easily distributable without need of refrigeration and safe. Trent thinks that probiotic E. coli-based vaccines could fit the bill.
“The bottom line is that we are not being responsible enough when it comes to antibiotic usage.”
– Stephen Trent, UGA Foundation Distinguished Professor, College of Veterinary Medicine
‘The Fight of Our Lives’
The cause of the antibiotic resistance crisis is multifold.
Industrial agriculture adds antibiotics to feed to keep animals in close quarters from getting sick but in doing so puts antibiotics into the meat people consume.
Some physicians prescribe antibiotics to patients with viral infections—despite antibiotics being ineffective against viruses—because patients expect to leave the doctor’s office with medication.
People feel better after a couple of days and stop taking antibiotics before their prescription actually runs out.
Mullis, however, strictly followed doctor’s orders. After months of applying ointments and a year of popping pills, his infection abated. He was lucky.
So, what’s the solution, if you can call it that?
Scientists have started “shelving” antibiotics, putting new antibiotics on hold until the next drug-resistant bacterium strikes rather than putting to immediate use. Physicians are being taught to use antibiotics only as a last resort and only for infections that are caused by bacteria and therefore respond to antibiotic treatment. Public relations campaigns in the United Kingdom and elsewhere abroad encourage citizens to use up their prescriptions and to be understanding when their doctors deny them one.
As for Trent, he’ll continue to look for the chink in the armor coating of bacteria, poking holes until he figures out how to break it open.
“The bottom line is that we are not being responsible enough when it comes to antibiotic usage,” he says. “We are in the fight of our lives against antibiotic resistance. But most of us don’t even know it.”

About the Researcher
Stephen Trent
UGA Foundation Distinguished Professor
Department of Infectious Diseases
College of Veterinary Medicine