The humble canine—stalwart, affectionate, devoted—has been humankind’s boon companion for thousands of years, and dogs need do nothing more to prove their worth. But they seem to have been saving their best trick. Scientists at the University of Georgia have found that dogs may be key to the next generation of human vaccines.
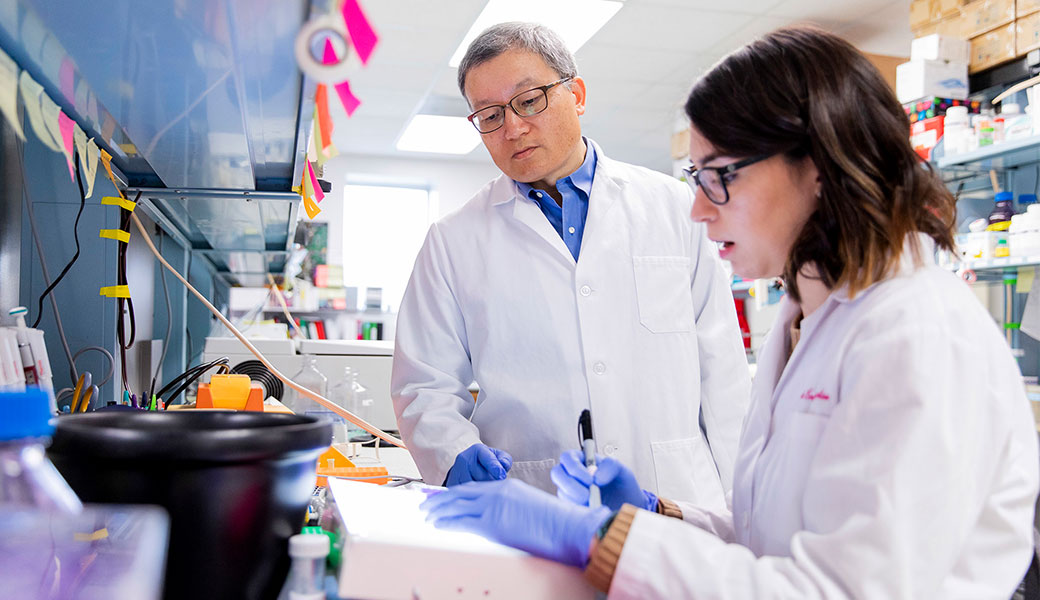
In truth, it’s not the dogs themselves, but rather a virus they carry and transmit that interests researchers. Called parainfluenza virus 5 (PIV5), it can cause respiratory illness in dogs but does not affect humans. Biao He, the Fred C. Davison Distinguished University Chair in Veterinary Medicine, has been studying this unusual virus for years, and he has successfully tested PIV5-based vaccines in animals, mostly on mice, against a range of diseases including influenza, rabies and even cancer.
Laced with promise
The allure of PIV5 is that in humans it is a relatively unobtrusive pathogen. Unlike some other viruses, which destroy host cells in the body and cause telltale signs of infection, such as hacking coughs and high fevers, PIV5 is readily detected by our immune system and quietly eradicated. If you ever acquire PIV5 infection, you’ll never know it.
Professor He and his colleagues exploit PIV5’s clandestine nature to their advantage by using it as a messenger that carries genetic information about diseases to the immune system without causing harm in the process. The scientists extract that information from a pathogen, attach it to PIV5 and turn it into an injectable or inhalable vaccine.
When this laced version of PIV5 enters the body, it is promptly disabled by the immune system, which in the process memorizes the unique genetic signatures of the pathogen and begins to develop antibodies that will protect against future infection.
None of this would have been possible had He not developed an interest in PIV5 and created a method of manipulating its genetic code when he was a postdoctoral researcher. “All my colleagues were working on really important pathogens like influenza at the time, and they would sometimes ask ‘Why are you bothering with a virus that doesn’t do anything?’” He said. “I had no idea that it would turn into a powerful vaccine platform, but I couldn’t do any of this work today if I hadn’t done the basic science first. Given the success we’ve seen so far, I’m glad I chose PIV5.”
Deadly diseases
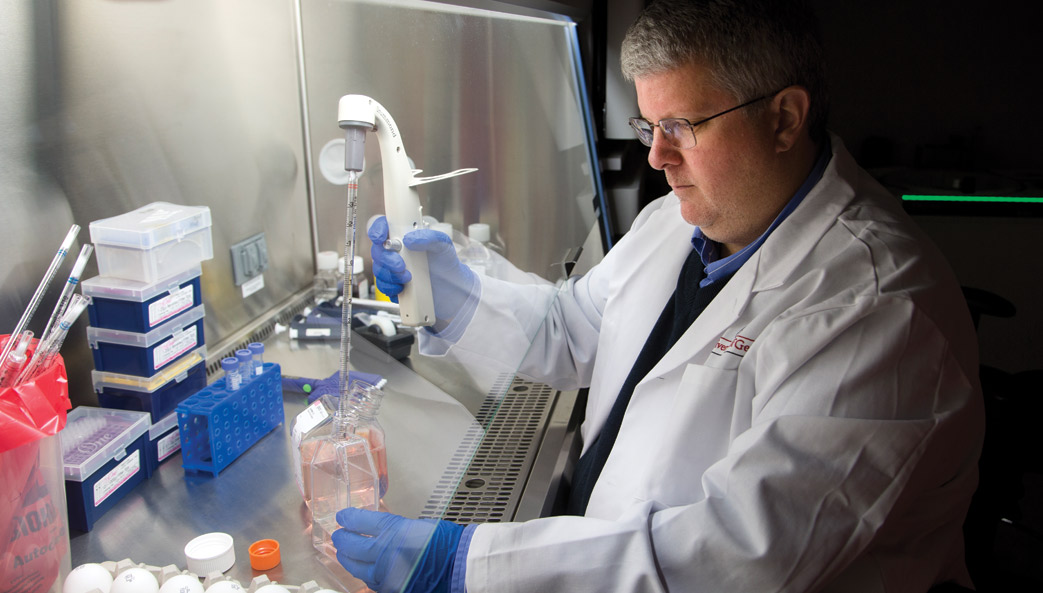
Working in partnership with Paul Spearman, professor of pediatrics and microbiology at Emory University, He is testing his PIV5 vaccine platform against one of the world’s most deadly pathogens: HIV.
While modern antiretroviral therapies can significantly extend the life of people suffering from HIV/AIDS, the disease still kills millions each year, and there are no vaccines approved to prevent HIV transmission.
“A vaccine is the holy grail in the fight against HIV,” He said. “But creating one is a daunting task. HIV is a tricky virus to work with, and our field is littered with failed vaccine attempts. However, Dr. Spearman and I are very optimistic about this new approach using PIV5.”
Spearman and He use a strategy known as prime-boosting to make their PIV5-based vaccine more powerful. The process involves priming the immune system by teaching it to target a specific antigen—the substance that causes your immune system to produce antibodies—and then boosting the immune response by re-administering the antigen again later.
The vaccine is designed to target very specific mucosal tissues, as previous studies have shown that HIV initially replicates in these tissues before spreading throughout the body via the bloodstream.
“In the past 30 years of HIV vaccine research, we have learned a lot about how to generate immune responses that might protect people from infection,” said Spearman. “We are optimistic that this prime-boost vaccine approach will generate immune responses to combat the virus in mucosal sites such as the gut. If successful, this will prevent the very early phase of HIV spread and could protect against HIV infection and AIDS.”
In another set of experiments, He is using PIV5 to create a therapeutic vaccine for rabies. Working with Zhen Fu, a professor of pathology in UGA’s College of Veterinary Medicine and internationally renowned rabies expert, He has created a new vaccine that shows great promise in mouse tests.
Successfully treating rabies can be a race against the clock. Those who suffer a bite from a rabid animal have a brief window of time in which to seek medical help before the virus takes root in the central nervous system. At that point, the disease is almost always fatal. “Basically,” said He, “the best way to deal with rabies right now is simple: Don’t get it.”
But in He and Fu’s mouse experiments, their PIV5 vaccine rescued many mice much longer after infection than what was previously thought possible. The animals were exposed to a strain of the rabies virus that generally reaches the brain of infected mice within three days. By day six, mice begin to exhibit symptoms that indicate the infection has become fatal. Yet 50 percent of mice treated with the new vaccine were saved, even after the onset of physical symptoms at day six.
“This is the most effective treatment we have seen reported in the scientific literature,” He said. “If we can improve these results and translate them to humans, we may have found one of the first useful treatments for advanced rabies infection.”
Apart from being effective in saving so many of the seemingly doomed mice, the PIV5 vaccine is also much safer than current treatments, which use a weakened version of the rabies virus.
“It doesn’t matter how much we weaken the current vaccine, because the virus inside is still rabies,” said Fu. “That is not a concern with our PIV5 vaccine.”

Influenza
Together with Mark Tompkins, an associate professor of infectious diseases at the College of Veterinary Medicine, professor He also tested a PIV5 vaccine designed to protect against H7N9 influenza, more commonly known as bird flu. H7N9 is one of several influenza virus strains that circulate in bird populations, with the first human cases reported in China in March 2013, according to the World Health Organization.
The H7N9 strain is of particular concern, however, because most patients rapidly develop severe pneumonia that sometimes requires intensive care and mechanical ventilation. “The mortality rate for this virus is over 30 percent, so there is an urgent need to develop a good vaccine,” He said. “Our PIV5 vaccine protected both mice and guinea pigs against a lethal H7N9 challenge, and we think
it may be a very strong candidate for human vaccine tests.”
Professors He and Tompkins also developed a PIV5-based vaccine for other forms of influenza. In mouse studies, this vaccine was 100 percent effective in protecting against H1N1, better known as swine flu, and the most virulent strain of H5N1, another form of bird flu. What’s more, the researchers think this platform could serve as a universal influenza vaccine.
Current influenza vaccines target viruses’ surface proteins. But because “these viruses change their surface proteins very easily,” He said, “at present we need annual vaccinations to match the circulating strains, and we depend on careful monitoring to make educated guesses about which versions of the flu will be most prominent every season.”
By contrast, the vaccine developed by He and Tompkins targets a protein inside the influenza virus called a nucleoprotein, which is critical for virus replication. Because nucleoproteins do not change as readily as surface proteins, the two researchers’ flu vaccine may protect patients against multiple strains for many years rather than just one year, He said.
RSV
In another set of experiments, He and UGA colleague Ralph Tripp, the Georgia Research Alliance Chair of Animal Health and Vaccine Development, have developed a new vaccine to protect against respiratory syncytial virus, better known as RSV.
Almost all children are infected with RSV by the time they are 2. Most recover quickly from the cold-like symptoms, but for others, RSV can lead to the development of bronchiolitis or pneumonia, which together land an estimated 75,000–125,000 American children in the hospital each year, according to the U.S. Centers for Disease Control and Prevention. Moreover, RSV is a major cause of morbidity and mortality among immuno-compromised adults and the elderly.
“Many have tried to develop an RSV vaccine, but they’ve been unsuccessful,” He said. “Our approach is different from all previous attempts, and now we have shown it works in animals.” In their experiments with mice, a single dose of He and Tripp’s PIV5-based vaccine protected the animals against RSV infection.
Their vaccine has another important key feature. Unlike infection by some other respiratory viruses, RSV does not induce long-lasting protective immunity against subsequent infection. “Our hope is that this RSV vaccine will protect people for life,” He said.“But even if it protects children and at-risk adults for only, say, five years, it will still be a big improvement.”
Creating a future free of disease
These are but a few of the projects that He has led since joining the University of Georgia in 2009. His laboratory is also exploring new PIV5-based vaccines for tuberculosis and malaria, among other diseases, and he has established his own startup company, CyanVac, to speed the movement of vaccine technologies into the marketplace—all from an unassuming virus that had been largely overlooked for years.
It seems only fitting that the world of science give back to those creatures that, however unwittingly, gave us this useful pathogen. Professor He got that opportunity recently when he devised a custom-made cancer vaccine for a dog suffering from soft-tissue sarcoma. After treatment with a PIV5 vaccine that taught the dog’s immune system to seek out and destroy the animal’s specific cancer cells, veterinarians were stunned by the result.
“The dog had an excellent response,” said Corey Saba, an associate professor of oncology at the College of Veterinary Medicine. “The tumor decreased in size by more than 50 percent and was not detectable on subsequent incisional biopsies.”
Despite his many successes, He is reluctant to say that he has found any cures, as a great deal of work remains to be done before most pets, much less humans, can get one of his vaccines from a doctor. But if his early results are any indication of what’s next, He and his colleagues may come to share the title of Man’s Best Friend with the traditional honorees.